About Us: Retina Times Retina Docs to the Rescue
============================================= -->Retina Docs to the Rescue
Elias C. Mavrofrides, MD, featured in RETINA TIMES, an official publication of the American Society of Retina Specialists (ASRS), Meeting 2017, Issue 70, Bridging the Past and the Future of Retina.
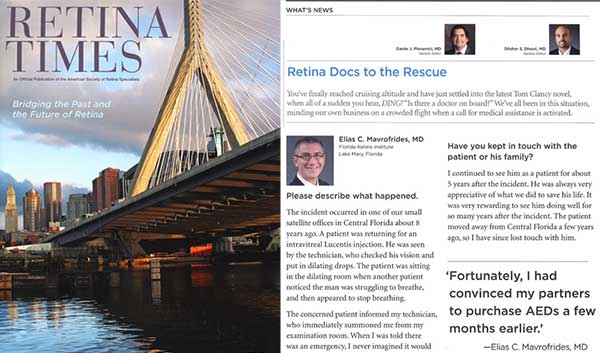
Please describe what happened.
The incident occured in one of our small satellite offices in Central Florida about 8 years ago. A patient was returning for an intravitreal Lucentis injection. He was seen by the technician, who checked his vision and put in dilating drops. The patient was sitting in the dilating room when another patient noticed the man was struggling to breathe, and then appeared to stop breathing.
"Fortunately, I had convinced my partners to purchase AEDs a few months earlier."
The concerned patient informed my technician, who immediately summoned me from my examination room. When I was told there was an emergency, I never imagined it would be anything this serious. I saw the patient sitting unconscious in the dilating room, and I was still hoping it would be a simple fainting spell. As I attempted to wake the patient, I realized he had urinated himself. The patient was not responding at all, so I quickly realized the gravity of the situation.
I calmly remembered to follow the ABCs— airway, breathing, circulation. I double-checked to confirm that he was not breathing and that there was no pulse. We then began administering CPR. Fortunately, I had convinced my partners to purchase AEDs a few months earlier. We quickly connected and initiated the AED, which confirmed that the patient was in cardiac arrest and provided initial an shock. When the patient did not regain a cardiac rhythm, we restarted CPR. A few moments later, the AED delivered a second shock— and the patient regained a regular cardiac rhythm and pulse.
Just as he regained pulse from the second shock, the paramedis arrived and further stabilized him. They subsequently rushed the patient to the closest cardiac ICU.
How did the patient do?
The patient survived the incident. In the cardiac ICU, he underwent further evaluation, and they confirmed an acute myocardial infarction related to severe coronary disease. He underwent coronary artery bypass surgery and made a full recovery. Within a few weeks, the patient was discharged from the hospital without any residual deficits.
Have you kept in touch with the patient or his family?
I continued to see him as a patient for about 5 years after the incident. He was always very appreciative of what we did to save his life. It was very rewarding to see him doing well for so many years after the incident. The patient moved away from Central Florida a few years ago, so I have since lost touch with him.
Did you feel prepared for the emergency?
Fortunately, I felt very prepared to handle the situation. During critical events like this, we realize the benefits of many years of medical training. And being a vitreoretinal specialist prepared me to be comfortable dealing with complex and intense situations.
We spend so much of our time in clinic making important decisions that have a huge impact on our patient's lives. Vitreoretinal surgery also teaches us to manage complex conditions with confidence and precision. So although I had never resuscitated a person before, I felt prepared because I had helped so many patients.
What was going through your mind during the event? Did time seem to slow down?
Yes, I experienced the sensation of time slowing down. When the incident started, everything seemed to be happening very quickly. I was initially in shock that something this serious was happening in my office. But once I realized he was in cardiac arrest, everything seemed to slow down. I have a very vivid memory of the entire event as if it were a movie.
Has the event changed anything in your life in anticipation that such a situation could occur again?
Now I pay even more attention when I take those CPR refresher courses. I also think the most important thing to consider is having AEDs more accessible. My request for our practice to purchase these defibrillators was based on what happened to a close friend of mine from high school, who was only 37 years old. A few months before the incident at my office, my friend suffered sudden cardiac arrest while coaching a high school basketball game. He was treated immediately by a physician in the crowd, but an AED was not readily available.
My friend was eventuelly resuscitated once the paramedics arrived, but it took over 20 minutes. Because he was pulseless for so long, my friend was left with a severe anoxic brain injury. This episode convinced me that we should have AEDs in our offices, considering that most of our patients are elderly and have multiple medical problems.
Is there anything you would have done differently?
Fortunately, everything turned out well and it seems that the decisions we made were good, so I would not have done anything differently.
Has this event changed your view of life?
This episode has definitely made me realize how fragile life can be. After the incident, I thought about the chain of events that occured for us to have been in a place to help that patient.
What if he hadn't had an appointment with us that day, and had suffered the cardiac arrest at home with no one to help him? What if the other patient in the dilating room hadn't realized something seemed wrong, and hadn't notified my staff right away? What if my friend had never had his incident, so I had never even thought to buy the defibrillators? What if my partners hadn't agreed to spend the money on the defibrillators, and we wouldn't have been able to resuscitate that patient so quickly? It's amazing to think of how many things had to align for us to be in a position to help this gentleman the way we did.